HEART DISEASE IS THE #1 KILLER IN THE UNITED STATES – MORE THAN ALL CANCERS COMBINED
I'm Sue Shershenovich & this is my story.
I’d like to share with you this journey and why LEOCADIA, INC is my way of raising money to help fund research and provide education regarding this very serious subject.
I always knew there was heart disease in my family history. During stressful periods my blood pressure would rise and eventually I started taking a low dose beta blocker (Atenolol) for that. I was overweight and had chronic indigestion/GERD along with chronic pain on the left side of my back by my shoulder (which I assumed was from sitting at a desk).
After I turned 53 I asked my primary care physician for a referral to see a cardiologist to determine a baseline for my heart health. After initial bloodwork, I learned my Total Cholesterol = 214 (optimal < 200), LDL = 111 (0ptimal < 100), HDL = 73 (optimal > 60), and Triglycerides = 162 (optimal < 150). The doctor suggested I lose some weight and if that didn’t work he would put me on a low dose statin and have my blood drawn again in 6 months. My blood pressure was normal, so he took me off the Atenolol and asked that I take my blood pressure daily and bring the results with me to my next appointment.
I’ve struggled with my weight for years and I heard myself say “is it okay if we skip the part about me trying to lose weight and go right to the statin?” I assured him I would still try to lose weight because I didn’t want to be overweight I just hadn’t found a way to successfully lose the weight. Six months later my weight was about the same and my cholesterol was now acceptable. My blood pressure daily log showed normal readings without medication. Life was good.
Fast forward two years and I’ve gained 15 pounds, in walks the doctor and the first thing he does is hand me a pedometer and suggests I try to walk 10,000 steps a day. He also asks if I would be open to a referral for a 6-month Cardiac Prevention Program where I would have appointments twice a month to help me with my weight loss and explains that it would involve meeting one on one with a nutritionist, exercise physiologist and a different cardiologist. Immediately I say yes.

First item is to get baseline bloodwork – Total Cholesterol = 171, LDL = 92, HDL = 65, and Triglycerides = 146. After the bloodwork is taken, I have my first appointment and meet the team. At my one on one meeting with the nutritionist I find out I will be keeping a food diary and that we will be reviewing it together at each visit. I find out what my calorie, protein and fiber goals are for each day. At my one on one meeting with the exercise physiologist I find out I will be keeping track of the number of steps I walk each day and that I should be walking a minimum of 10,000 steps each day and that we will be reviewing my log together at each visit. Finally, I meet with the new cardiologist and she explains that the lifestyle changes I’ll be making through diet and exercise will be reflected in the next blood draw.
The first month was a real struggle. Getting used to writing everything down – and being truthful about what I ate. I gradually worked up to 10,000 steps a day but then it was an effort to stay at 10,000 or above every day. I needed the accountability and dreaded it at the same time. The easy part was meeting with the cardiologist because her piece didn’t kick in until the blood draw. I still had an exam and was asked if I was in any pain.
THERE ARE STILL MANY UNKNOWNS - ESPECIALLY REGARDING WOMEN'S HEART DISEASE AND CORONARY MICROVASCULAR DISEASE
Click here to read “The Secret of the Small Arteries”
by UC Irvine Health
At one appointment with my cardiologist, I mentioned that I had read women’s heart disease sometimes presented different than men’s heart disease. That it could present as indigestion. I mentioned that I have had indigestion/GERD for about 20-25 years and asked “how would I know if what I’m feeling is really indigestion or if it could be heart disease”?
A series of questions followed, she wasn’t sure if it was heart related or not or if I needed to see a gastroenterologist. Then, a request for another log – when does it happen and what is going on right before it happens. I explained it’s most of the time, that nothing really triggers it and that it can wake me up from sleeping in the middle of the night.
At my next appointment, we reviewed my log. As a result, she suggested an EndoPAT to rule out any heart related issues. An EndoPAT is a non-invasive test that measures changes in function of the arteries. The EndoPAT took 15 minutes and at the end of the test the nurse asked about my next appointment. Due to the holidays I, wouldn’t see the doctor for at least 3 weeks. The nurse left and within 5 minutes, the doctor walked in with the nurse to tell me that it was an abnormal EndoPAT and now she knew for sure there was something wrong with my vascular system.
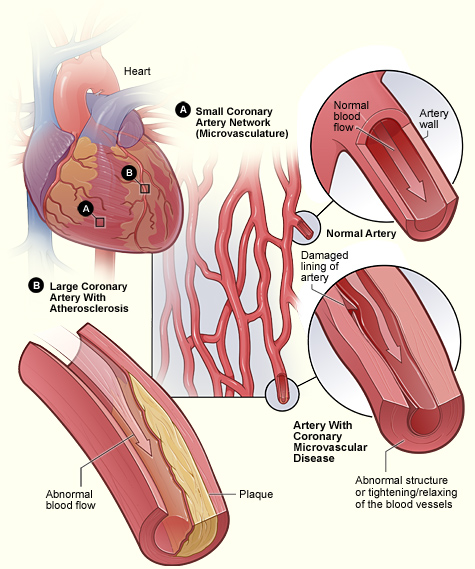
The next test I had was the Coronary Reactivity Test(CRT). The CRT is an invasive test, an angiogram, that examines how blood vessels in the heart respond to different medications which helps determine whether the microscopic size arteries are working normally.
Test results showed that I have “coronary microvascular disease” or MVD. MVD or “small vessel disease” was once thought to be a rare condition, but the numbers are much greater than originally thought. I now take medication and no longer experience chronic indigestion/GERD (which I learned was Angina) and no longer experience the chronic pain on the left side of my back by my shoulder (which I learned is a symptom of women’s heart disease). After 6 months in the Cardiac Prevention Program I lost 30 pounds and my Total Cholesterol = 174, LDL = 83, HDL = 79, and Triglycerides = 108. The change in lipids over 4 months was due to lifestyle changes only – diet and exercise changes only. I continue to wake occasionally in the middle of the night with chest pains (angina).
When I wake during the night I feel chest pains, pain on the left side of my back by my shoulder or sometimes jaw pain, sometimes nauseous, and sometimes clammy. An episode can last up to 30 minutes. I use nitroglycerin spray for relief and generally that works.
To date, I’ve only had to call 911 once as I had 2 incidents within an hour. The result was a type of heart attack known as a coronary artery spasm, silent heart attack, unstable angina, or heart attack without blockage. It happens when one of the heart’s arteries tightens so much that blood flow stops or becomes drastically reduced. There is no permanent damage during a coronary artery spasm. While silent heart attacks aren’t as serious, they do increase your risk of another heart attack or one that may be more serious.
I continue in a monthly Cardiac Rehab Group and have a one on one appointment with my cardiologist on a regular basis.